WHEN TRYING FOR A BABY, HOW LONG SHOULD I WAIT BEFORE I WORRY ABOUT NOT GETTING PREGNANT?
It is very difficult to be specific. One in five women falls pregnant within a month of starting to try.
After six months of having sex without contraception, seven out of ten women have conceived.
After a year, approximately 85 per cent of women will be pregnant and after two years, the figure is 95 per cent.
AT WHAT STAGE SHOULD COUPLES FAILING TO CONCEIVE DECIDE TO SEE A DOCTOR?
Most doctors will not send you for tests until you have been trying for at least a year. Unless you have a specific medical problem.
Women under 35: it is reasonable to try to get pregnant for 12 to 18 months before going to see the doctor.
Women over 35: Seek help after six to 12 months because fertility treatment success rates decline quite rapidly with age.
WHAT CONDITIONS COULD AFFECT MY FERTILITY?
Women: Lack of periods and irregular periods. Pelvic surgery (burst appendix, for example), pelvic infections and sexually transmitted infections such as Chlamydia,, very heavy and painful periods.
Men: Testicles didn’t drop when you were a child, visible varicose veins on your scrotum, surgery such as hernia repair, trauma, or a sexually transmitted infection.
WHAT EFFECT DOES AGE HAVE ON A WOMAN’S FERTILITY?
Natural fertility begins to decline when a woman is in her late twenties and her chance of conceiving declines more rapidly each year.
At the age of 35 women are about half as fertile as they were at the age of 25, and by the age of 40 they are about half as fertile as they were at 35.
DOES A MAN’S AGE AFFECT HIS FERTILITY?
Men produce sperm well into their seventies but the quality of it deteriorates after they are about 45.
WHAT FERTILITY TESTS ARE THERE FOR WOMEN?
Ovulation Test: The majority of women who have regular periods will be ovulating (releasing an egg each month). The usual test for ovulation is a blood test. This measures the level of the hormone progesterone and the blood sample is taken a week before a period is due.
A further blood test: If a woman is over 35 and has been trying for more than two years, or has irregular cycles, a blood test between days three and five of her menstrual cycle is helpful. This measures the follicle stimulating hormone (FSH). If the level of FSH is raised this may be a sign that she is about to start the menopause.
Tubal potency: An x-ray called hysterosalpingography (HSG) can tell if the Fallopian tubes are blocked or damaged. It is done in hospital or laboratories and takes about 20 minutes. The patient does not need a general anaesthetic but the procedure can be painful.
Doctors also test your tubes with ultrasound, using a special fluid to show up any blockages.
Ultrasound scans: These can pick up problems in the womb such as fibroids (fibrous lumps) and measure the lining of the womb. This needs to be thick if you want to get pregnant.
A scan can also measure the development of follicles – sacs which contain eggs – in the ovaries to see if they are growing properly, to check for polycystic ovaries (PCO) or polycystic ovary syndrome (PCOS). Too many cysts on your ovaries can affect fertility. IVF success rates for women with PCO are very high.
Laparoscopy: This procedure is usually carried out under general anaesthetic. A tiny camera is inserted through the belly button to view the uterus and dye is inserted into the cervix to check the fallopian tubes for blockages.
This test is offered to women who have risk factors such as pelvic inflammatory disease or blocked tubes, a history of endometriosis or Chlamydia, women over 35, or those who have been trying for a baby for more than two years.
WHAT ARE THE TESTS FOR MEN?
Sperm test or semen analysis: Analysis of a sample can discover sperm concentration (sperm count), the motility of sperm (swimming ability) and the morphology of sperm (shape and structure). It can also identify infections and antibodies.
WHAT FERTILITY TREATMENTS ARE AVAILABLE?
Intra-uterine Insemination (IUI): This is worth trying before you go for IVF, especially if sperm quality is below average or you have “unexplained infertility” which is where no medical reason for failure to conceive can be found. It is often used to insert donor sperm and it is only suitable for women with healthy fallopian tubes.
A woman’s cycle is monitored to predict the day that her egg will be released and drugs may be used to stimulate the ovaries to produce more than one egg in the normal menstrual cycle. Sperm is then inserted into the womb at ovulation using a catheter (this has been called the turkey-blasting method) which maximizes the chances of fertilization taking place.
Success rates vary between 12 and 15 percent per cycle, depending on a woman’s age but after six cycles of the treatment more than six out of ten patients will have become pregnant.
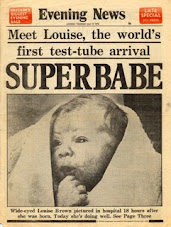
In Vitro Fertilisation (IVF): This is the procedure classically known as the test tube baby technique. There are five stages to IVF as follows:
1. Down regulation: So called because the woman is given drugs (such as Buserelin or Naferelin) which shut down her ovaries so her cycle can be carefully controlled. This will put her into a temporary menopause.
You can have an injection of the drug once a day in your buttock or thigh. They can be given by a nurse or your partner – or you can do it yourself. If you are squeamish about needles you can use a nasal spray to inhale the drug several times a day but this is more expensive than injections. You do this for two to three weeks. But be warned – you will feel as if you have PMT to a factor of ten.
2. Egg production: you then add a second injection of drug called human menopausal gonadrotophin (HMG), a hormone highly purified after being taken from pregnant women’s urine, or FSH. This stimulates the ovaries to produce several egg-containing follicles rather than the one that would happen naturally. During this process you will be carefully monitored by ultrasound and will feel quite bloated but not as bad-tempered as in Stage One.
3. Egg collection: when the follicles reach the right size and maturity you will be given an injection of human chorionic gonadatrophin (HCG). This mimics the surge in hormone which normally triggers ovulation. Thirty-five hours later the eggs are collected, either by laparoscopy or via the vagina, before they have the chance to move down the Fallopian tubes naturally.
The operation is carried out under general anesthetic or vaginally under sedation and may leave you feeling sore. The more eggs that are collected, the more painful it can be but it increases the likelihood of success.
4. Fertilisation: at the same time the eggs are collected, the man has to provide a sperm sample. The eggs and top-quality sperm (200,000 sperm per egg) are placed in a glass dish by an embryologist. If successful, fertilization will take place within 24 to 48 hours and throughout this period you will be feeling tearful and anxious.
5. Embryo transfer: the two best quality (fertilized eggs) are put back into the womb via a catheter. You may be offered progesterone to increase your chances of getting pregnant.
This experience is an emotional rollercoaster. You and your partner will have an anxious two-week wait to find out whether the embryos have become implanted and you are pregnant.
Unfortunately, hormone levels caused by the drugs can make you feel pregnant even if you are not. So if you are unsuccessful the arrival of your period can be even more devastating than normal. Success rates on average are 25 per cent per cycle.
Intracytoplasmic Sperm Injection (ICSI): This is a way of fertilizing eggs by injecting a single healthy sperm into an egg by using a glass needle that is one-fourteenth of the thickness of a human hair.
As with IVF, the woman takes a course of drugs before collection of the egg. ICSI is used where the man has a low sperm count or fertilization is a problem. It costs (£5,000) about N700,000 which includes IVF treatment and the drugs you need.
ivf slidestory:
Monday, November 23, 2009
Subscribe to:
Comments (Atom)